Seniors deserve timely access to care, not bureaucratic hurdles | Viewpoint
Congress needs to pass legislation to streamline the prior authorization process so patient care isn’t delayed. The measure has bipartisan support.
Like most doctors, I’m awed by the transformative power of medicine in my patients’ lives. Yet, I’m also frustrated that insurers are increasingly delaying or denying necessary care.
That’s because doctors’ ability to provide procedures and medications is hampered by the bureaucratic nightmare that is prior authorization built into many Medicare Advantage plans.
Prior authorization, which requires doctors to jump through numerous administrative hoops before insurance companies approve necessary treatments, impacts every specialty in medicine.
But what’s worse is that many of these adverse events could have been prevented entirely. In 2022,
What can go wrong with the prior authorization process? Consider
For many seniors, getting cataract surgery can mean the difference between living independently and relying on others for help with daily tasks like driving, cooking, or walking. Peggy Mitchell, a Medicare Advantage beneficiary from Alpharetta, was forced to
After a long appeal process, the denial was eventually overturned, but not before her MA plan’s policy had already caused tens of thousands of other cataract surgeries to be canceled. While her insurer eventually
In fact, many other insurers erect similar barriers that prevent patients from getting the cancer, rheumatology, substance use disorder, and other care they desperately need. As a result, the Kaiser Family Foundation estimates
The administrative burden of prior authorization doesn't just impact patients; it also strains our healthcare system. All the time spent battling insurance companies is time taken away from patient care. Doctors and their staff are forced to dedicate valuable resources to navigate the labyrinth of an approval process, diverting them from their core responsibility – providing quality care.
This costs practices money that they would much rather invest in direct patient care and forces them to hire staff solely dedicated to managing the overwhelming amount of paperwork insurers require. It's unacceptable that insurers are requiring physicians to complete unnecessary, extensive, burdensome paperwork that insurers then use to overrule physicians’ clinical judgment and trusted relationships with patients.
Ultimately, when coverage for medically necessary care is denied, patients are forced to forgo care altogether or pay for treatments out of their own pockets, often at great expense. In fact,
And now, with the rise of AI, I’m even more concerned as
Americans have had enough. It’s time we address this rampant problem.
With time running out in the 118th Congress, I urge lawmakers to quickly pass
- Establishing an electronic system: Eliminating the antiquated fax system and mandating electronic submission of documents would streamline the process and reduce errors that delay care.
- Increasing transparency: There is currently a lack of available data about MA claim denials. This bill would require plans to submit more detailed data to give patients and providers more transparency throughout the entire process.
- Speeding up decisions: By clarifying the Center for Medicare & Medicaid Services’ authority to establish timeframes for e-prior authorization requests, patients enrolled in MA plans will be able to get the care they need quicker.
The Improving Seniors’ Timely Access to Care Act recently reached a major milestone: It now has 50 cosponsors in the Senate and more than 218 in the House of Representatives. Everyone knows modernization of the prior authorization process is long overdue. That’s why lawmakers on both sides of the aisle and hundreds of healthcare organizations are all in agreement.
It's time for Congress to finish the job. Pass this prior authorization bill before the end of the year.
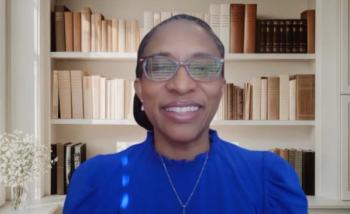
Jane C. Edmond, MD is the president of the American Academy of Ophthalmology.