- Politics
- Diversity, equity and inclusion
- Financial Decision Making
- Telehealth
- Patient Experience
- Leadership
- Point of Care Tools
- Product Solutions
- Management
- Technology
- Healthcare Transformation
- Data + Technology
- Safer Hospitals
- Business
- Providers in Practice
- Mergers and Acquisitions
- AI & Data Analytics
- Cybersecurity
- Interoperability & EHRs
- Medical Devices
- Pop Health Tech
- Precision Medicine
- Virtual Care
- Health equity
Nonprofit hospitals are faring better, but ‘not out of the woods’
Even with signs of improvement, health systems still face headwinds. Suzie Desai of S&P Global Ratings provided an overview for hospital executives.
Seattle - Nonprofit hospitals may be seeing a little less difficulty financially than they did a year ago, but they continue to face formidable headwinds.
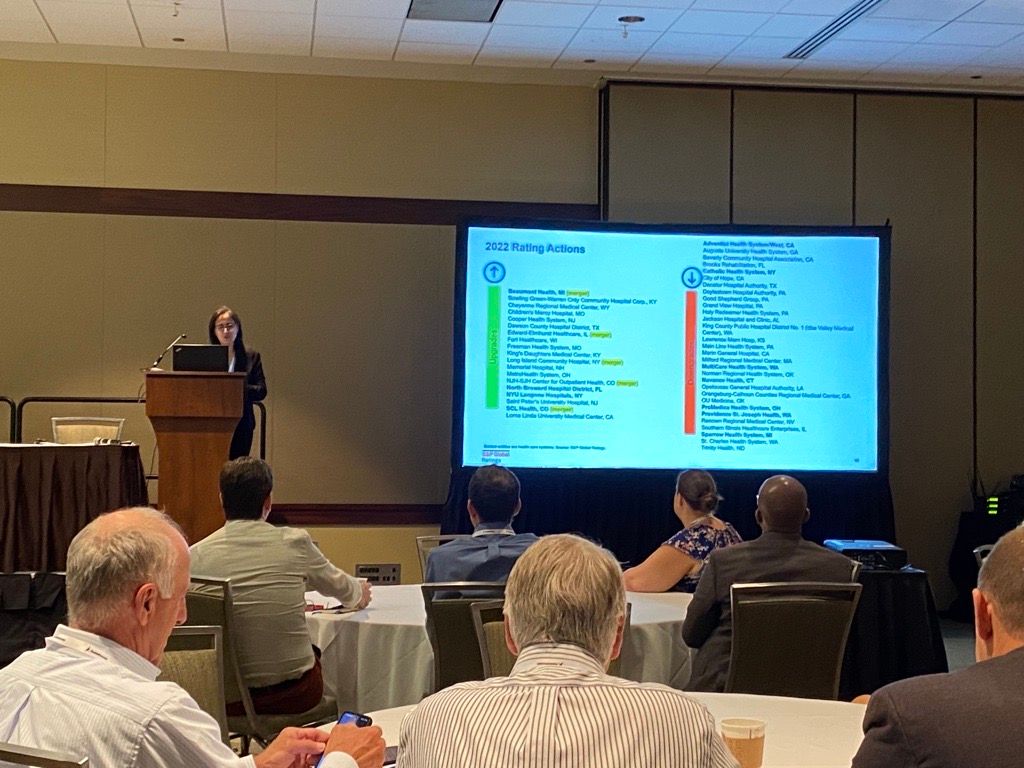
Suzie Desai of S&P Global Ratings outlined some of the challenges for nonprofit hospitals at the American Hospital Association Leadership Summit. (Photo: Ron Southwick)
Suzie Desai, senior director and sector lead of the U.S. nonprofit healthcare group of S&P Global Ratings, says there are still signs of trouble as she outlined the financial landscape during the American Hospital Association Leadership Summit this week.
“We’re not out of the woods,” Desai said.
But she said the pace of the recovery of the hospital sector remains an open question.
For most hospitals, 2022 was the worst financial year of the pandemic, according to Kaufman Hall, a healthcare consulting firm. About half of America’s hospitals ended the year with negative operating margins.
Last year, S&P Global Ratings assigned a negative outlook for the nonprofit hospital sector. The firm is in the midst of analyzing data for 2023, but she told the audience that it’s possible that the nonprofit hospital sector will continue to have a negative outlook for investors this year.
So far in 2023, S&P has given ratings downgrades to 21 hospitals, while eight hospitals have received upgrades. Desai noted that some hospitals received changes in ratings due to mergers and acquistions, and she also said S&P placed a priority on examining hospitals that have been having more difficulties.
Health systems continue to wrestle with labor challenges, Desai says. It is encouraging that nonprofit hospitals are relying a bit less on temporary staffing agencies to fill openings for nursing jobs and other roles, noting that both usage and pay rates have dropped. However, hospitals continue to turn to staffing agencies “more than they did in the past,” Desai said.
She also notes that turnover remains “stubbornly high.”
Unions have also been more aggressive in demands for better compensation for their workers, and those contract talks could result in higher expenses for hospitals.
Hospitals also continue to deal with higher costs for supplies, and some analysts have noted that the rise in prices for some goods has been a headache on par with labor expenses.
Payer reimbursement rates continue to lag, which has proven to be another drag on hospital finances, Desai said.
On the upside, health systems have fared better with their investment portfolios in 2023, which has been a stabilizing factor. She also noted that hospital volumes have rebounded. Many patients deferred treatment during the worst of the pandemic, health system officials say, but industry analysts say more people are seeking care.
“We're generally seeing good volumes,” Desai said.
Still, hospital volume takes on increasing importance as hospitals wrestle with higher labor costs and inflation. With health systems facing higher expenses, their operating margins are increasingly dependent on treating a higher volume of patients.
Revenues have not rebounded to keep pace with expenses. Desai noted that S&P places a high value on how much cash on hand hospitals are maintaining.
In looking at other risks, Desai notes that cybersecurity attacks, while not threatening all health systems, can be costly to health systems. Hospitals are also seeing higher insurances costs for cybersecurity as well, she said.
Cybersecurity experts say they’ve seen an uptick in data breaches and ransomware attacks in recent months. This month, HCA Healthcare reported a cyberattack that could have affected as many as 11 million patients.
Some hospitals continue to house patents longer than they would like, partly because nursing homes and other post-acute care facilities aren’t able to take them due to their own staffing woes. The “length of stay” continues to be an issue for some hospitals, Desai said.
More hospital mergers have been taking place in recent months, which is another trend worth watching, she said. This year, Kaiser Permanente announced its plans to acquire Geisinger Health, and she also pointed the merger discussions of UnityPoint Health and Presbyterian Healthcare Services.
“This area does seem a little more active than after the last year and a half,” Desai said.
