How a public hospital improved nurse retention
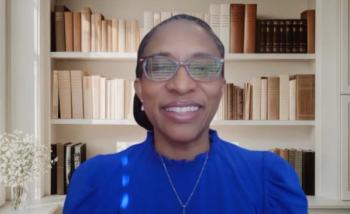
Nancy Blake, chief nursing officer of Los Angeles General Medical Center, talks about creating a better work environment and keeping more nurses in the hospital.
Very few public hospitals have received the Magnet designation from the American Nurses Credentialing Center, which recognizes hospitals providing top-notch care and meeting high standards in nursing.
This year, the Los Angeles General Medical Center received that honor. It signifies a remarkable effort to improve the work environment for nurses, which has resulted in improved retention and reduced turnover.
Nancy Blake, chief nursing officer of Los Angeles General Medical Center, joined the hospital in 2021 with hopes of achieving Magnet designation. She tells Chief Healthcare Executive® that it required new approaches from nurses and leadership.
“It was a whole culture change,” Blake says.
“I knew that there were a lot of structures and processes to be put in place,” she explains. “I also knew that the leadership culture needed to change, and their approach towards staff definitely needed to change in order to improve retention.”
The medical center has found new success in holding onto younger nurses. The retention rate of nurses two years after graduation surged from 35% to 91%. The turnover rate, which was 22% in 2021, has dropped below 10%.
“To actually get below 10% at a public county hospital is phenomenal,” Blake says.
Blake talks about the effort to change leadership approaches, moving to a shared governance model, and empowering nurses.
As she looks back on the effort, Blake says, “Their needs were not insurmountable. They wanted someone who listened. They wanted someone who advocated.”
(See part of our conversation in this video. The story continues below.)
Being servant leaders
Blake says it was critical to galvanize leaders to embrace a different approach to working with nurses.
“We are servant leaders,” she says. “The staff don't report to us. We report to the staff, and our job is to eliminate all the barriers and to listen to them.”
The medical center implemented a residency program and took other steps to help new nurses, including moving more nurses from the bedside to help train younger nurses and give them a better chance to succeed.
As a public hospital, the medical center isn’t going to fare as well in compensation as other hospitals. Blake points out the medical center offers good benefits and a pension plan, although she says younger nurses aren’t so focused on retirement planning.
But Blake says the hospital has focused on making sure nurses see enticing career possibilities.
“We will help you get where you want to get,” she says. “If you want to be a nurse practitioner, you come in … be a good nurse for a few years. And we have nurse practitioners in our system.”
The hospital has lost some nurses who are seeking better pay, but some of those have ended up returning to the medical center.
“Probably the best marketing tool I have is to have those people come back after six months and say, ‘You know what, the grass is not greener,’” Blake says.
The medical center has also focused on identifying nurses with leadership potential. The hospital launched a leadership development program that focuses on servant leadership and communication.
"We've done a lot of things to ... make sure that you're not just promoting somebody because of their clinical skills and then they fail as a leader, but you're teaching them how to be a good leader as well," she says.
Empowering nurses
The hospital also moved to a shared governance model, giving nurses a stronger voice and the ability to make decisions. While Blake still has to make some decisions, teams of nurses now have the authority to make choices and more freedom in management. When doctors approach Blake about plans to make a change, Blake directs the physician to talk with the different committees involved, such as the professional practice committee.
“They really feel empowered to make decisions,” Blake says.
Nurses also manage their own scheduling. They have to work a certain number of weekends and ensure that there are enough nurses with certain competencies on each shift, but they can switch shifts and generally handle their own schedules. Younger nurses in particular crave that flexibility.
Blake says she’s also worked to give nurses the ability to speak more freely. When she arrived, Blake says nurses viewed the environment as “punitive.”
Now, more nurses feel respected and believe that leaders care about them and their patients, Blake says.
Blake hosts a regular chat with nurses to talk about what she is working on and to hear their concerns. Still, she says it took time to convince nurses that they could talk about problems that needed to be resolved.
“I think, after probably a year, they trusted that there wasn't going to be ramifications if they spoke up, if there was a true, genuine issue on their unit,” she says.
“If you don't tell us, we can't make it better,” Blake says. “And if you think we know, because you guys are all chatting about it, you're sadly mistaken. You've got to let us know what we can do.”
‘We need to listen’
Blake says a critical component of engineering the turnaround at Los Angeles General Medical Center involved adopting the American Association of Critical-Care Nurses’
“Everything was based around the healthy work environment standards,” Blake says.
The AACN developed
“We saw an increase in each and every one of those areas,” Blake says.
Blake says one area where the medical center is working to improve is providing meaningful recognition to nurses.
“I think this newer, younger generation wants to be acknowledged for the little things that they do,” Blake says. “They always feel very important when somebody acknowledges those little things. And somebody said, ‘It's like they really care about us, and they really know what's going on.’”
Vicki Good, chief clinical officer of the American Association of Critical-Care Nurses, says the turnaround at Los Angeles General Medical Center shows that all hospitals and health systems can make changes to improve the workplace for their nurses. She notes it shows providers with modest budgets and even public hospitals can do better for their nurses.
“They were able to take it within their own hospital and say, Okay, these are the things within our parameters of control, and these are the things that we're going to change,” Good says. “So no matter how system-based your hospital is, there's certain things within your control, and how you act on those things within your control, really is how you make a difference in your work environment.”
In the intensive care unit, Blake deployed more nurses. While California has a minimum staffing law for its hospitals, Blake recognized that more nurses were needed in the ICU because the patients were sicker.
The healthy work standards were deployed across the medical center’s system, including clinics and the nursing unit in the county jail.
The medical center has gained a big return on its investment in nurses, particularly by keeping more of its nurses on staff. The hospital is not spending as much time and money training and retraining replacements, Blake says.
Blake stresses the importance of communicating with frontline nurses.
“We need to listen to the staff, and we need to retain them, and we need to find out what's important to them,” Blake says.
She recalls the day the hospital received the call about winning the Magnet designation.
“We had a conference room that normally holds about 200 people seated,” Blake says. “We had about 400 people in there. Many of them were staff nurses, and I just wanted to cry when I saw how excited they were, because so many people had told them, ‘You're a county hospital, you can't do it.’”